The power is in your hands
Post date: 01/06/2013 | Time to read article: 5 minsThe information within this article was correct at the time of publishing. Last updated 18/05/2020
In April the clinical landscape of the NHS will undertake the biggest change since its inception in 1948. In his analysis of the changes, Dr Simon Abrams raises concerns over potential conflicts of interest.

On 1 April this year a national experiment in health redesign will take place. Every birth and death and every healthcare intervention will be affected as accountability for commissioning health services will pass from managers to clinicians for the first time.
It begs the question: will the changes in the health and Social Care Act move healthcare forward in this country?
The birth of CCGs
Most CCGs have been authorised. For many this authorisation demanded a real change in primary care involvement. Clinical engagement is a precondition and when it is not there the National Commissioning Board has demanded better.
As never before, GPs’ email boxes are full of regular updates, information about healthcare changes, requests for agenda items for neighbourhood practice meetings – all calling on frontline GPs to involve themselves in the wider issues of local healthcare. CCGs are meeting to identify healthcare priorities using public health data.
General practice is being asked to examine its performance from the inside out. Why are diabetes complications high? Why are spirometry levels low? Why are alcohol-related admissions high? More importantly, doctors are being asked what can be done about it.
CCGs are working with GP colleagues to reduce inappropriate referrals, leading to healthcare savings.
Opportunity or black hole?
Historically, doctors are more interested in looking after patients than health politics. These changes will create opportunities and risks. Under the previous system, NHS managers were accountable to their line managers, then to the NHS Executive and central government. A command and control system was in place where health service policies were decided centrally and implemented.
CCGs are now accountable to grassroots GPs. The BMA called for GPs to closely scrutinise the constitution. That scrutiny needs to continue to ensure that CCGs make decisions that lead to improved patient care. If local GPs are concerned that their CCG is making the wrong decisions, they must hold them to account.
The opportunities are there for local GPs to seek health service changes relevant to their population. If CCGs want to maintain their authority they must commission health services along lines that maintain local GPs’ confidence.
"If local GPs are concerned that their CCG is making the wrong decisions, they must hold them to account"
Previous attempts to engage clinicians in strategic planning had limited success – for example, the professional executive committees of the PCTs.
Once on the respective professional executive committee, many GPs lost contact with their professional colleagues. Whilst they often did good work, primary care did not move with them. Clinicians with operational experience who move to strategic positions on the CCGs, whilst at the same time remaining accountable to their primary care colleagues, is a cause for relative optimism.
At a glance
Conflicts of interest need to be managed effectively by Clinical Commissioning Groups (CCGs). For a GP a conflict of interest may arise when their own judgment as an NHS commissioner could be, or could be perceived to be, influenced by their own concerns and obligations as a healthcare provider. However, with good governance and planning CCGs should be able to mitigate these risks.
Handling conflicts of interest
Will the relationship between leading and following GPs stand up? Will it turn into an “us and them” view? A major factor will be the handling of conflicts of interest. Those in a CCG are GPs with enthusiasm and drive to make a difference; these people have opportunities to both commission and provide, so conflicts of interest are inevitable and need to be managed effectively by CCGs.
For a GP a conflict of interest may arise when their own judgment as an NHS commissioner could be, or be perceived to be, influenced by their own concerns and obligations as a healthcare provider.
"Those in a CCG are GPs with enthusiasm and drive to make a difference; these people have opportunities to both commission and provide, so conflicts of interest are inevitable"
Avoiding accusations of conflicting interests will require a declaration, both through a register of interests, and appropriate behaviour when commissioning decisions are being made. With good governance and planning CCGs should be able to mitigate these risks.
Conflicts of interest do not in themselves suggest impropriety. It is the impropriety that is the problem. CCG members must remember that impropriety must both be avoided and seen to be avoided.
Impact on secondary care
What about secondary care? One piece of advice was about the number of conversations between primary and secondary care clinicians. Before Choose and Book, lifting the phone to discuss management of a complex patient was not unusual. The practice has diminished. The anonymous referral is standard. Choose and Book provides email advice services, but anonymity of professionals remains. GPs no longer attend grand rounds.
Yet the subtleties of healthcare are better communicated in dialogues between GPs and consultants. Implementing more community-located consultant clinics might contribute to the reestablishment of the dialogue, and as part of the out-of-hospital strategy, will be a natural way to progress.
Regulation
"For the dedicated innovators, opportunities will arise to do things differently and more effectively"
The changes have led to new statutory bodies responsible for different parts of the NhS, with the NHS Commissioning Board as the main overseeing body. Decision-making processes of old have gone and new ones are yet to be set up. For some this will mean inertia and limit progress. For the dedicated innovators, opportunities will arise to do things differently and more effectively.
The Health and Social Care Act established Health and Wellbeing Boards. Their role is to implement the Joint Strategic Needs Assessment of the local population including both health and social care. It is taking a while for them to apply their influence, but this may change in the future.
Privatisation
A concern over the White Paper was privatisation damaging healthcare. The Francis report has shown that excessive focus on targets can also cause damage. Bringing the private sector into health has led to the development of a series of vibrant social enterprise services. Currently 46% of patients in England and Wales have out-of-hours primary care delivered by social enterprises.
"There is growing evidence that many of these providers are performing at a standard higher than daytime general practice"
Despite early criticism there is growing evidence that many of these providers are performing at a standard higher than daytime general practice. They certainly work to more stringent performance requirements.
The future
The Francis Inquiry recently identified endemic problems in the health service that will fluently cross the switch from PCTs to CCGs and remain unless addressed. Such problems include the silo working that enabled poor practice to be ignored by some professional groups, the culture of gagging those who want to speak out and the problems of services being run by staff for the benefit of the staff rather than patients.
An NHS accountable to GPs at the frontline of care should be able to recognise what is good and develop it and what is not working and change it: the process should be approached with cautious optimism.
Event
Dr Abrams is the keynote speaker at the MPS Out of Hours Conference on 25 April 2013 in London. He will be talking about taking the temperature of the NHS.
To find out more visit www.medicalprotection.org/uk/events
Three second survey
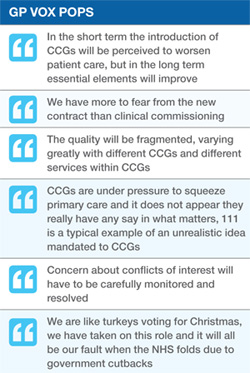
What effect do you think the introduction of Clinical Commissioning Groups (CCGs) will have on patient care?
- I expect it will improve patient care – 29.61%
- I expect it will worsen patient care – 27.86%
- It won’t affect patient care – 15.03%
What are your concerns about the introduction of CCGs?
- Budget restrictions – 79.74%
- Time constraints – 66.36%
- Conflicts of interest – 58.85%
- Quality of care – 31.9%
- Other – 14.3% (including practice workload increase, fragmentation).


