“Respect for the autonomous choices of persons runs as deep in common morality as any principle.” –
TL Beauchamp and JF
Childress, Principles of Biomedical Ethics (2001)
Compliance is generally considered to be when a patient‘s behaviour adheres to a clinician’s recommendations. This is quite a clinician centric concept and so it can be helpful to consider whether talking about a concordant patient is more appropriate, which is one where the patient’s personal views and choices have been considered and respected, and the clinician and the patient have agreed a management plan together. This plan may not be exactly what the clinician would have recommended, but indicates a compromise between both parties
What is the doctor’s role?
A doctor’s primary concern is to do their best for their patients; this includes giving advice and treatment, and arranging investigations in accordance with the current evidence base and the patient’s best interests.
Why can non-concordant patients present difficulties?
All practices will have a cohort of patients whose autonomous choices conflict with the suggested course of action of their doctor. Given that there is no obligation to provide a treatment requested by a patient that is not to their overall benefit, this can give rise to clashes between doctor and patient.
What are the commonest scenarios in relation to non-compliance?
- A patient has been started on a treatment, but declines to attend for subsequent review and/or monitoring checks. This scenario puts a GP in an invidious position, in that a decision has already been taken that it is in the patient’s best interests to commence a particular treatment. This can create a new risk that must be balanced when judging what is in the best interests of the patient.
- A patient who declines the investigation or treatment of symptoms with a potentially serious and/or treatable underlying cause.
Key points
It is important to remember that it is unlikely that a doctor will be legitimately criticised if a competent patient has made an informed decision to pursue a particular course of action.
The Medical Council states that you must respect and support the patient’s right to seek a second opinion or to decline treatment, or to decline involvement in education or research.
If a shared understanding is reached between the doctor and the patient, it can be a positive experience in which both parties can feel heard and respected and the compromise reached is one that both are content to follow .
To protect themselves a doctor must be in a position to justify the approach taken, and to demonstrate that they made the patient clearly aware of the risks of non-compliance. Comprehensive records are essential.
If a patient is declining a treatment which a doctor feels is clinically necessary the doctor should document
- The choices of treatment which have been offered to the patient
- The pros and cons of each treatment option
- The possible adverse consequences if the advice of the doctor is not followed and how likely this adverse outcome is
- That the patient has been offered further information on the matter or possibly a second opinion
- Discussion with the patient regarding whether or not the treatment option will still be available in the future
- What the patient’s decision is and if possible what reasons the patient gives for that decision
- That the clinician believes or has evidence that the patient is competent to refuse treatment
- That it has been made clear to the patient that they are free to come back and discuss the options further
- Consider arranging follow up or setting a recall, so that the issue can be raised again with the patient at a later date.
If a patient is refusing a treatment it is important to always consider whether the patient is competent to make that decision. If there is any question as to the patient’s competence then this should be looked into further and the possibility of a psychiatric review should be considered.
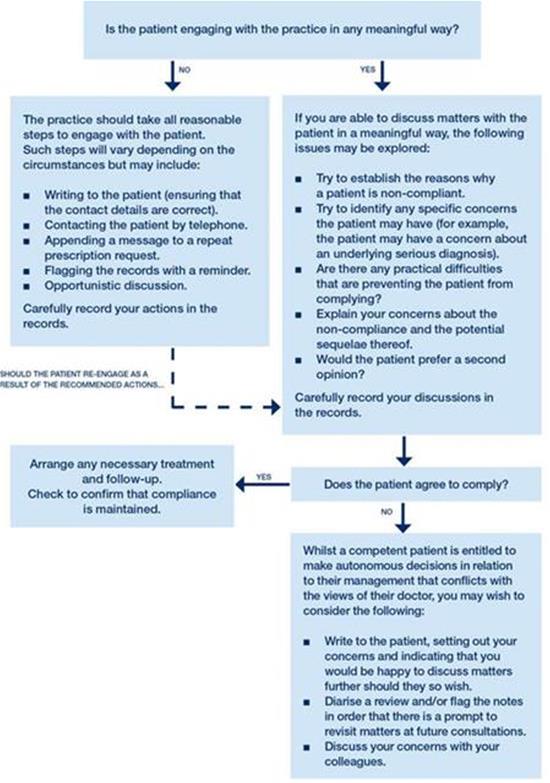
You should end your professional relationship with a patient only when the breakdown of trust means you cannot provide good clinical care. For a diagramatic view of the step-by-step approach to management of a non-compliant patient, please see the flowchart below.
This factsheet is aimed at providing general advice only. We encourage any member who needs more specific advice about the risks associated with a patient who is refusing treatment, or refusing monitoring, to contact one of our medicolegal consultants at Medical Protection on 0800 2255677.
Step-by-step approach to dealing with non-compliant patients:
Further information
Good Medical Practice (paragraphs 31 to 34)