Learning from cases: Psychiatry
Post date: 09/07/2025 | Time to read article: 6 minsThe information within this article was correct at the time of publishing. Last updated 15/07/2025
Read this resource to:
- understand the claims environment in psychiatry: Insights and lessons learned
- receive tailored advice and key recommendations to help you reduce risks in the future
______
Psychiatry is a unique field, so the advice you receive needs to be equally specialised.
As a Medical Protection member, you benefit from more than 130 years of experience defending doctors and other healthcare professionals. That isn’t just a number – it’s more than 13 decades of specialist expertise that we use to protect you long into the future.
The team at Medical Protection, including medicolegal experts and cases and claims specialists, have delved into a huge range of psychiatric cases to analyse the common reasons for claims and the different case types, to help keep you up to date with the current trends and provide insights into the psychiatry claims and complaints landscape.
We hope you find this a useful source of guidance and advice, empowering you to protect yourself throughout your career.
Introduction
As a psychiatrist, you are used to working in complex and pressured environments and navigating risk. We also know, following feedback from members, that experiencing a medicolegal case can be incredibly stressful. At Medical Protection, we want to share our knowledge, experience, and expertise with you so we can provide invaluable professional support.
Analysis
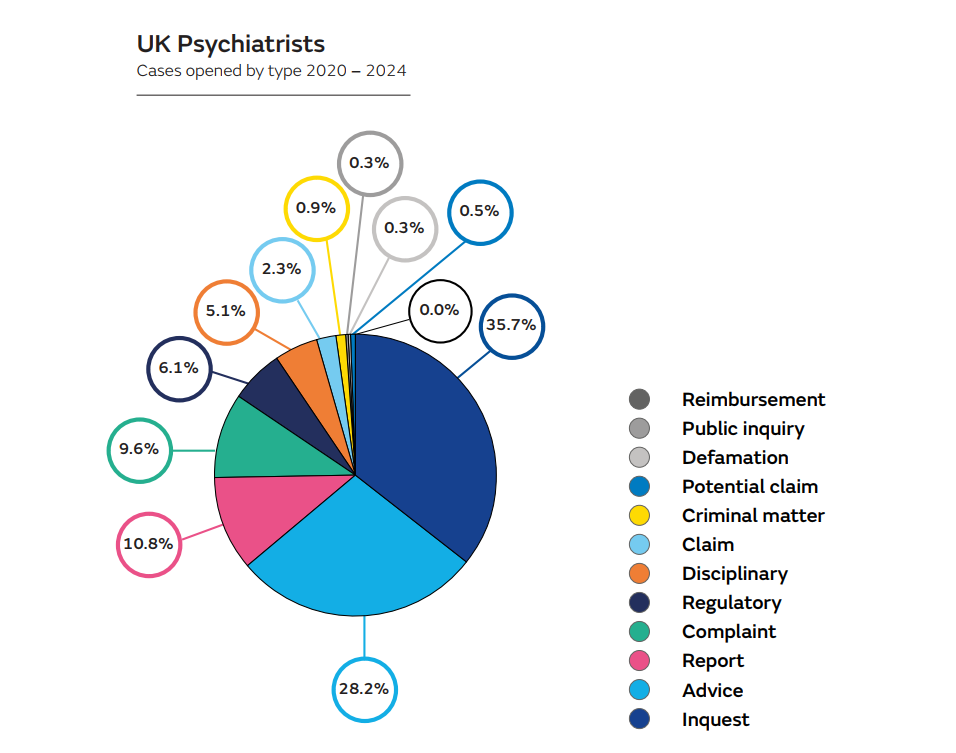
We have analysed the support we’ve provided UK-based psychiatrists between 2020 and 2024 – over 2,000 cases. In addition to providing medicolegal advice and assistance in writing medical reports in over 900 of these cases, we have supported our members through over 1,400 situations, including:
- claims, defined as demands for monetary compensation that embody allegations of negligence
- potential claims, defined as intimations from a claimant of a possible claim for compensation
- complaints
- General Medical Council (GMC) investigations
- local disciplinary procedures
- inquests
It is also not unusual for more than one medicolegal process to arise from a single incident or complaint, either simultaneously or successively, each with their own process and possible consequences – a concept called multiple jeopardy. A clinician may, for example, be subject to an inquest, clinical negligence claim, and GMC investigation relating to the same case, meaning potentially years of stress.
Claims: procedures and contributory factors
The value of a settled claim will often include compensation for care and loss of earnings if applicable, in addition to an award for the damage that resulted from a breach of duty. The value of each claim varies enormously, with our payment (including damages, costs, and legal costs) considered in this analysis ranging from tens to hundreds of thousands of pounds.
By reviewing the claims cases, including those defended, not pursued, and settled, we’ve identified some of the reasons that patients take action against psychiatrists.
The following themes of claims opened over the past decade were identified:
- Alleged negligent management of both informal and detained patients, in particular with regards to risk assessments prior to leave and regarding observation levels, as well as failure to admit patients, leading to attempted or completed suicide.
- Delays in management of physical health conditions while an inpatient.
- Alleged inappropriate long-term prescription of medications that can cause dependence or inappropriately rapid tapering of medication.
There were also some claims brought against psychiatrists acting as expert witnesses, alleging their expert evidence was inaccurate, leading to harm or financial loss.
Patient complaints: common themes
More than 200 complaints were analysed, covering a wide range of concerns and reflecting the range of issues a psychiatrist can face. Complaints were received both about work in the NHS and in the private sector, and included the following themes:
- Attempted or completed suicide following consultations or during inpatient stay.
- Breach of confidentiality/data by disclosure of patient information without appropriate consent to GP, social services, school, employer, to the incorrect healthcare professional, the other parent, or even patient correspondence sent to incorrect address.
- Inaccurate or incorrect psychiatric reports, particularly for children and for neurodevelopmental disorders.
- Complaints regarding diagnoses being reached or not reached, including parental disputes.
- Inaccurate or inappropriate clinical records, including errors in correspondence to GPs or discharge letters, inappropriate wording or tone in letters, and the extent of detailed history included in certain parts of record such as care plans. At times, these complaints include a request for notes to be deleted or amended.
- Communication, for example not explaining side effects of medication appropriately.
- Manner and attitude, such as allegations that the psychiatrist had a dismissive, unprofessional attitude, and patients feeling that insufficient time was spent with them and not feeling listened to.
- Disputed DVLA notification/referral.
- Clinical allegations, for example inappropriate prescribing or tapering of medication, and lack of liaison with other healthcare professionals leading to delay in treatment.
- Difficulty accessing clinic appointments and obtaining prescribed medication.
A significant proportion of the complaints related to medical records, including inappropriate disclosure without patient consent, and concerns being raised about the content of the records or reports. Of those assessing and managing children, parental disputes over reports, diagnoses, and management were not uncommon.
Regulatory (GMC) and disciplinary cases: common themes
We are aware of the immense pressure and stress that many doctors go through during these investigations. We always aim to provide members with tailored care and expert support.
GMC cases and hospital disciplinary matters have followed concerns raised by patients, relatives, or colleagues, both senior and junior. There was a mix of clinical and non-clinical concerns. Some investigations related to more than one concern or a series of serious clinical incidents. The common themes were:
- Clinical performance concerns, such as inappropriate prescription, diagnosis and management, failure to assess patient before Section 17 leave, failure to warn about medication side effects, improper monitoring of physical side effects of psychotropic medication, suicide following discharge, and unjustified section.
- Probity issues, such as private or locum work while on sick leave, or retrospectively amending medical records.
- Inappropriate behaviour towards colleagues and patients.
- Health issues, including alcohol or drug misuse.
- Personal conduct, for example following criminal convictions, such as for driving offences.
- Concern or criticism of expert witness work.
In the absence of representation by a defence organisation, the cost of instructing a solicitor to assist with a regulatory matter can be significant, and this may be substantially higher if other case types are also involved, such as disciplinary action or an inquest.
Inquests: common themes
We assisted members in writing statements and attending coroners’ inquests on over 800 occasions between 2020 and 2024. An inquest is a factfinding exercise that is conducted by the coroner, and, in some cases, in front of a jury. The purpose of an inquest is to find out who died – when, where, how, and in what circumstances. In some circumstances, such as in cases of unnatural deaths in those detained under the Mental Health Act, the inquest will be held with a jury.
Further information about what happens at an inquest and what to expect can be found in our essential guide to inquests.
Our analysis identified the following themes:
- Suicide of patients in the community, including shortly after discharge from hospital or while waiting for inpatient care to be arranged.
- Suicide of hospitalised patients while on unsupervised ward leave, following absconsion from ward or absconsion from escorted ward leave, informal patients leaving the ward without agreement, and reduction in observation levels.
- Deaths in a prison setting.
- Deaths from deterioration in physical health while on an inpatient ward – such as from sepsis.
- Deaths from recreational drug misuse/overdose and alcohol misuse.
- Inquests involving victims of homicide, allegedly perpetrated by psychiatric patients.
We have also advised on providing a statement where the psychiatrist was involved in resuscitation attempts taking place on inpatient wards.
Most inquests conclude uneventfully, but if a clinician is criticised by the coroner during the inquest or in the conclusion, then it is usually necessary to self-refer to the GMC to fulfil the obligations imposed by Good Medical Practice.
Read related case report - Good records in a worst-case scenario
Psychiatry in the UK: top tips to minimise risk
Please note this is not an exhaustive list of recommendations, but key learning points from our analysis.
- Be mindful of the information included in medical records and clinical reports, ensuring they are accurate with clear sources of information, as well as using appropriate tone and language. It may be helpful to review this with the patient when appropriate to check they are satisfied with it.
- Accurate and clear documentation, which often may need to be relied on years after the event, is the cornerstone of any medicolegal defence.
- Be particularly careful when sending documents including patient information and ensure they are sent to the intended recipients. Medicolegal advice can be sought for third party requests for confidential patient information.
- Ensure patient reviews and risk assessments are conducted thoroughly and documented clearly. Including the decision-making process and explanations for decisions made is also extremely helpful.
- Take extra care regarding the physical health complaints of hospitalised patients, seeking specialist input if needed.
- Understand your patient’s concerns and expectations and address any queries they may have.
- Some complaints brought by patients or relatives follow dissatisfaction with the manner and attitude of their psychiatrist. Pay attention to how you may be perceived during discussions and ensure time is taken to explain the situation and answer any questions.
- Demonstrate empathy in your consultations and show your patient that they are the focus of your attention.
- Carefully discuss carefully the management plan regarding medication, particularly with regards to possible side effects and check for understanding.
- Be aware that you may be asked to write a statement, including in relation to claims, inquests, and complaints about your practice months or even years after an event, and ensure that your contemporaneous record keeping would allow you to give a comprehensive account of your involvement, even if you cannot remember the patient concerned.
- In the event you have concerns about either your own or your colleague’s fitness to practise (for example, for health reasons) you should seek advice.
- Ensure you are fully indemnified to carry out the full scope of your practice in the UK, including medicolegal or expert witness work.
- Seeking advice early when confronted with a situation that is challenging or complex from a medicolegal perspective can reduce the chance of a complaint escalating or even arising in the first place.
About the author
Dr Sara Sreih trained in psychiatry before joining Medical Protection in 2016. She initially handled cases for members in England and Wales, before moving to support members in Asia, the Caribbean and Bermuda with both claims and cases.
