Avoiding a ‘near hit’
Post date: 06/04/2013 | Time to read article: 7 minsThe information within this article was correct at the time of publishing. Last updated 18/05/2020

Clinical Risk Manager Julie Price shares simple tips for handling test results
“Dr Black, I came to see you two months ago and am still feeling unwell. I saw the nurse for the blood tests you ordered and phoned for the results a few days later as requested; the receptionist told me they were all normal so I just don’t understand why I feel so tired?!”
Dr Black reviewed Susan’s computer record, accessing the results of her blood tests. Most of the results were normal, but there was one showing abnormalities – the thyroid function test. Dr Black knew immediately what had happened. He had brought this issue up many times at practice meetings, ie, relying on the patient to telephone the practice for their results. Susan had telephoned after a few days, but the TFT results took longer to be returned.
Dr Black explained the oversight to Susan, offering an apology. He diagnosed primary hypothyroidism and prescribed thyroid replacement therapy.
“Phew,” thought Dr Black, “No harm done then, but a near miss, or perhaps more accurately a near hit!” Dr Black recorded this incident on the practice significant event form and sent it to the practice manager to be included at the next SEA meeting. He knew the practice test result system was flawed.
Practices use the laboratory services on a daily basis, sending off specimens and receiving results, which are checked for abnormalities and actioned as necessary. Is the system you have at your practice robust, effective and safe? When was the last time a test result was lost or not conveyed to a patient? Can you be sure that there are no reports in the system that you have not seen or acted upon?
Like many risks in general practice the effective management of test results is threatened by both a lack of robust systems and human error. Welldesigned test results systems can trap human errors and help reduce the likelihood of adverse events, thus preventing harm to patients.
An MPS study found that approximately 60% of claims in general practice handled by MPS related to the failure to diagnose. Many of these can be attributed to system error, eg, an abnormal test result not acted on; a test result scanned into the wrong patient record, or an abnormal result not communicated to the patient.1
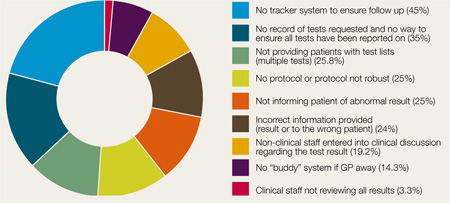
Figure 1: Test result risk
% of practices visited with this risk
What are the risks?
Over the past nine years MPS has conducted more than 1,000 Clinical Risk Self Assessments (CRSAs) in general practice. The data analysing from 120 CRSAs conducted during 2012 reveals that 87.9% of practices had risks associated with their test results system. Figure 1 highlights the key risks relating to test results.
RISK 1: No tracker system to ensure follow up
The request for follow up may be made because the practitioner has identified a suspicious symptom, wishes to reexamine the patient, wants to review the progress of the presenting complaint, or review the patient’s symptoms when the results of the tests are available.
What may be of concern to the practitioner is that there is no reliable method of checking that the patient has attended his/her follow-up appointment. A lack of appropriate follow-up may lead to a delay in diagnosis.
Introducing either a manual or computerised “tracking system/log” allows for effective tracking of patients the practitioner feels requires monitoring or follow up.
The tracker log allows clinicians to enter patients they are particularly concerned about. Fortnightly or monthly, a nominated receptionist collects the logs and checks that the patient has attended for follow up; the name can be then removed from the log. Alternatively, the receptionist can inform the practitioner that the patient has not been followed up. The log could look something like Figure 2.
Figure 2
*Only the first three columns are filled in by the practitioner
RISK 2: No record of tests requested and no way to ensure all tests have been reported on
One of the challenges for practices is ensuring that all the samples that are sent off to the laboratory are returned as results. Clearly, if results that are normal are lost, this is unlikely to be of clinical significance, but abnormal results could be important.
Practices may consider undertaking an audit of “ins and outs” of patient samples sent to the laboratory, including blood tests and microbiology samples, to ensure that all results are returned. Some computer software programmes now have an electronic pathology test requesting system. This is a reliable method of tracking ins and outs, allied to barcode identification of samples and requests.
RISK 3: No system for dealing with multiple tests
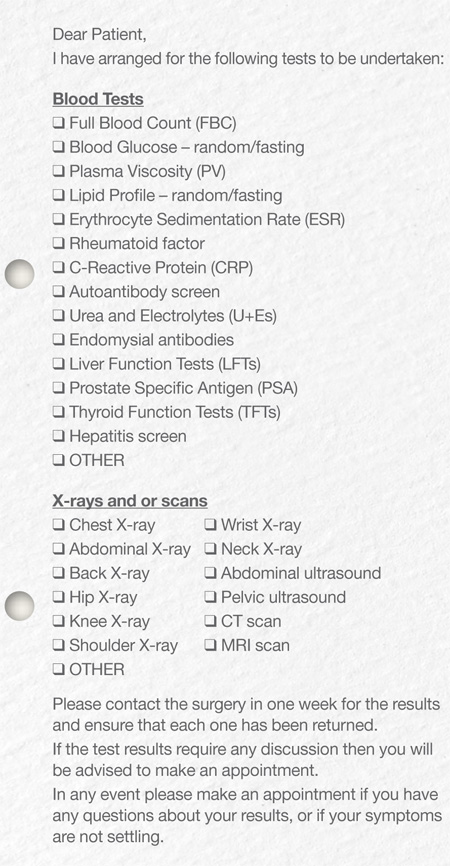
The patient should be informed of how many tests will be carried out. Consider providing patients with a list of the samples that they have had taken (tick box on a pre-printed sheet) along with the usual time scale.
RISK 4: No test result protocol
All practices should discuss and draw up a protocol for dealing with test results which includes three key elements: testing, processing the results and actioning. The protocol should be read by all relevant members of the practice and signed to confirm that this is the case.
RISK 5: Patient not informed of abnormal result
Responsibility for actioning results lies with the practice. Practices could develop a proactive system for dealing with abnormal results, minimising the risk of a test result being overlooked. It should not be assumed that the patient will phone up the practice to find out if any action is necessary following tests, as many will not do so for a variety of reasons.
The practice should endeavour to offer and encourage patients to attend for appropriate reviews and investigations. For patients who repeatedly DNA these appointments, the practice needs to demonstrate that they have taken all reasonable steps to contact the patient and explain the implications of the results.
Record all attempts. It is important to remember that some patients may be less able to take responsibility for their health than others, for example, those with learning difficulties, communication difficulties, cognitive impairment or mental illness. Do not file a result unless it has been actioned.
Normal results may prompt an action as well as abnormal results, for example, a patient with a normal ferritin result may be in a position to cease iron therapy. Similarly if the hospital have asked the GP to follow up results, whether copied or not, the GP should ensure that the results are obtained and appropriate action taken.
Figure 3: Example of a multiple test sheet
RISK 6: Giving out the incorrect result, eg, result from a different date or incorrect patient
Prior to giving out a test result, confirm the patient’s identity using three identification markers, ie, name, address and date of birth. Clarify the nature of the test results and the date on which they were taken. Encourage patients to keep their contact details up-to-date – the time of referral is an ideal time to confirm details.
RISK 7: Non-clinical staff entering into clinical discussions about the results
The reception staff should not enter into any clinical discussion about test results, but simply read out the doctor’s comments. These should be simple and unambiguous so that the receptionist reading them out is less likely to be asked further questions about the result by the patient.
If further discussion is needed, a telephone appointment should be made with the doctor. There may be some results that should always be conveyed by the doctor (for example, malignancies, HIV tests). Consider developing a traffic light system:
- Green results are those that can be conveyed by the receptionist, practice nurse or GP
- Amber results are those that can be conveyed by either the practice nurse or GP
- Red results are those that can be conveyed by the GP only.
RISK 8: No “buddy” system if GP away
A buddy system should be in place so that no results are missed when staff are on holiday or sick leave, or are absent from the practice. Ensure there is such a system in place whereby when a clinician is not available another GP checks the results, thus making sure no urgent abnormal results are overlooked, or the necessary immediate response delayed.
RISK 9: Clinical staff not reviewing all results
In 3.3% of the practices visited, the clinician only reviewed test results marked as abnormal, owing to time constraints. All other results were sent to the patients’ records unread. This system is unsafe. Clinicians should review all test results.
Finally
It is essential that a practice has a robust and effective test result system and that all staff are fully trained in the procedure. However, no system is ever foolproof, and if an adverse event or ‘near hit’ does occur, the practice should discuss this at a significant event meeting. Lessons should be learnt and the protocol reviewed to prevent a repeat occurrence, thus avoiding potential harm to patients.
References
1. Silk N, What went wrong in 1,000 negligence claims? Health Care Risk Report(2000)
Dilemma
What should staff do if someone other than the patient answers the phone when they try and relay a test result?
 Test results, and doctors’ messages about those results, should only be transmitted to the patient and not to relatives or other individuals without the patient’s consent. Develop a simple consent form which would give permission for a relative (of, for example, an elderly patient) to be able to discuss certain issues with the practice on the patient’s behalf, eg, test results, repeat prescriptions.
Test results, and doctors’ messages about those results, should only be transmitted to the patient and not to relatives or other individuals without the patient’s consent. Develop a simple consent form which would give permission for a relative (of, for example, an elderly patient) to be able to discuss certain issues with the practice on the patient’s behalf, eg, test results, repeat prescriptions.
This form, once completed by the patient, should be scanned into the patient’s record and a note made on the computer so that it is visible when a family member speaks to the practice. The practice should ensure that all staff are aware of the forms and that they can only discuss medical information with a third party within the confines of the consent that has been provided. Consent should be revisited at reasonable intervals, or if further investigations are ordered.
