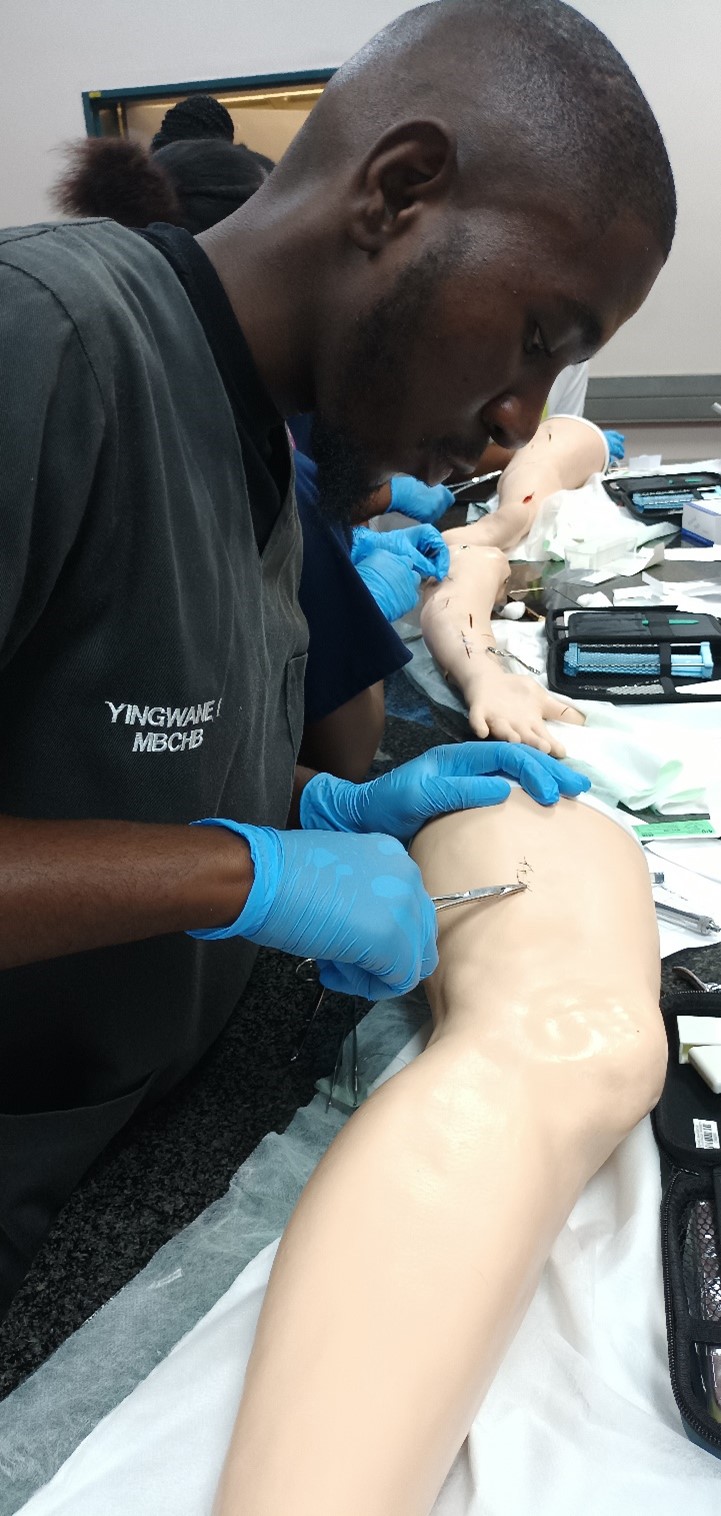
As a fourth-year medical student, Ikaneng Yingwane gives his advice around informed consent, and always keeping it front-of-mind when dealing with patients.
______
The concept of informed consent is taught to us (health sciences students) from the first year, and in the subsequent years, it is reiterated to make sure that it becomes a part of our daily practice. However, the art seems to be lost in some of us when it comes to the application of the theory. We tend to dive right into taking the patient history and examining them without knowing if the patient fully comprehends everything that would be taking place. Other times we do not attempt to explain what is it that we will be doing with the patient, and that could potentially impact patient care negatively. The problem in obtaining proper consent lies in the blurred lines between implied and informed consent.
Implied consent is consent that is not given explicitly but can be inferred based on a patient's actions. We tend to take a patient's compliance as a sign that they have consented to be examined. Though time effective, it is ethically unacceptable because the patient’s autonomy is compromised in the process. On the contrary, informed consent is obtained when a patient is made aware of processes that about take place from history taking to the risks and benefits of the interventions involved.
In order to obtain adequate informed consent, one needs to be patient-centred first, and not apply the same formula for each consultation. When explaining the procedures and treatment, it should be done in a language which the patient can understand, and the details need to be outlined thoroughly. The patient should be given the opportunity to ask questions should they arise during the session, and in answering one ought to be truthful, and answer as fully as the patient wants (and if possible, provide answers that are in line with recent literature). Throughout the consultation, one needs to ascertain if the patient understands the information that is being provided.
One needs to explain to the patient if a follow-up visit is necessary and advise on the availability of counselling and support services if any. Towards the end of the consultation the patient should be advised that they have the right to seek a second opinion with regard to the outcome of the consultation, this further reaffirms patient’s autonomy.
Informed consent is vital in a consultation setting and should precede any interaction between healthcare professionals and patients. It should be well documented, whether in writing or recorded. It is an art that ought to be practiced religiously to improve patient care and satisfaction. The regular practice of obtaining informed consent will ensure that the theory is not lost on us in consultation with patients.
______
To read more student articles like this visit our student hub.