Read this resource to:
- understand the claims environment in dermatology: Insights and lessons learned
- receive tailored advice and key recommendations to help you reduce risks in the future
Expert advice for dermatologists
Dermatology is a unique field seen in both primary and secondary care, as well as presenting with significant overlap alongside other medical conditions, so the advice you receive needs to be equally specialised.
As a Medical Protection member, you benefit from more than 130 years of experience defending doctors and other healthcare professionals. That isn’t just a number – it’s more than 13 decades of specialist expertise that we use to protect you long into the future.
The team at Medical Protection, including medicolegal experts and cases and claims specialists, have delved into a huge range of dermatology cases to analyse the common reasons for claims and the different case types, to help keep you up to date with current trends and provide insights.
We hope you find this a useful source of guidance and advice, empowering you to protect yourself throughout your career.
Introduction
While dermatological complications may appear less likely than other medical specialties to lead to medicolegal claims, cases in dermatology are, in fact, relatively common. This is often due to the chronic nature of skin conditions, their visible consequences, or complications arising from treatment.
Dermatology is a fiercely competitive medical specialty, offering clinicians the opportunity to combine medical training with surgical skills. Data from a 2024 workforce survey indicated that there were 1,340 consultant dermatologists on the GMC specialist register, out of over 110,000 doctors on the specialist register in total.
As dermatology can be practised as a standalone specialty, or as a specialist area with general practice, it can be difficult to analyse the difference between cases that affect those solely practising dermatology and those who provide a more varied primary care service.
However, we do see a significant number of cases arising from primary care relating to delayed diagnosis in skin cancers, with malignant melanoma featuring in a number of cases.
As NHS Resolution manage claims relating to NHS patients in both primary and secondary care, most claims reported to us relate to private provision of dermatology, often due to long NHS waiting times.
The value of the settled claim will often include compensation for care and loss of earnings, in addition to an award for the damage that resulted from a breach of duty. The value of each claim varies enormously with our highest dermatology total case payment considered in this analysis (including claimant damages, costs, and legal costs) being over £1 million.
As a dermatologist, you work in a varied specialty where patients may be seeking cosmetic results as well as disease modification. We also know, following feedback from members, that experiencing a medicolegal case can be incredibly stressful. At Medical Protection, we want to share our knowledge, experience, and expertise with you so we can provide invaluable professional support.
Analysis
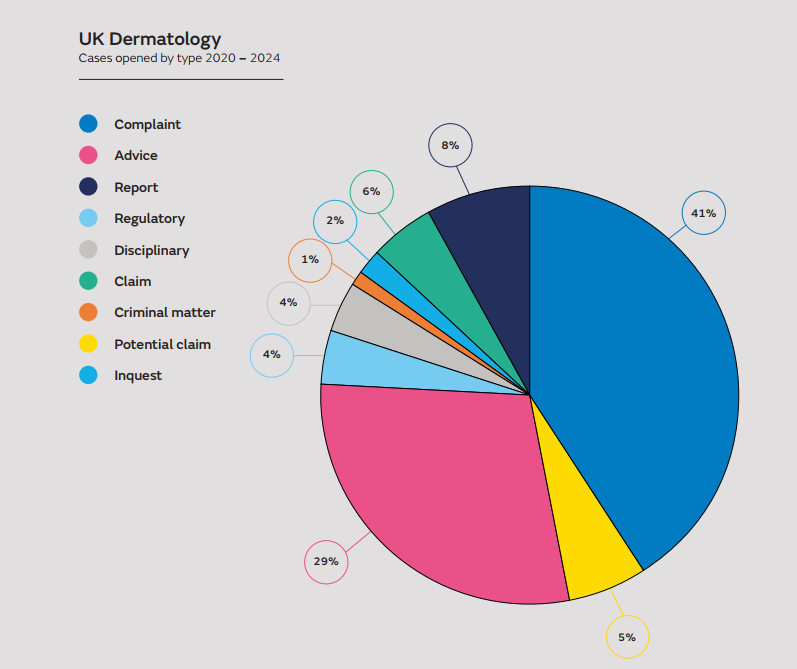
We have analysed the support we provided to UK-based dermatologists and primary care dermatology cases between 2020 and 2024 – in excess of 300 cases. We have supported our dermatology members in a full range of situations, including:
- claims, as in demands for monetary compensation that embodies allegations of negligence
- potential claims, which are intimations from a claimant of a possible claim for compensation
- complaints
- General Medical Council (GMC) investigations
- local disciplinary procedures
- inquests.
By reviewing all the claims cases, including those defended, not pursued, and settled, we’ve identified some of the reasons that patients decide to take action against dermatologists. Here you’ll also find some explanations of why claims are settled.
Claims: procedures and contributory factors
Not all claims are settled, and many potential claims do not develop into a full clinical negligence claim.
Where claims are settled, the settlement takes into account multiple factors that may not be limited just to the breach of duty stated by the claimant. Often poor record keeping can expose the clinician to significant vulnerability in medical negligence claims.
Delayed diagnosis
The most expensive claim case settled in the period reviewed related to a seven-month delay in diagnosis of malignant melanoma. While melanoma is the fifth most common skin cancer type, it only accounts for around 5% of all cancers, yet accounted for nearly 10% of claims and potential claims reviewed in this analysis. Delay in diagnosis can have significant implications for treatment options and significantly increased morbidity and mortality.
When assessing a lesion, there needs to be sufficient detail in records to understand the clinical rationale behind decision making. Although a subsequent statement or narrative can help to explain, vulnerabilities in contemporaneous medical records can often make it hard to defend a claim.
Dermatoscopy findings should be clearly recorded and consideration given to any information provided in a referral, especially where the features may have changed over time.
While delayed diagnosis for basal cell carcinomas is associated with less severe clinical outcomes than in malignant melanomas, it can still lead to the need for more extensive surgery, with greater scarring and psychological impact than would otherwise be the case. This accounted for all of the claims of this type.
Other dermatological conditions with delayed diagnosis and treatment that resulted in a claim included paraneoplastic dermatological features, squamous cell carcinoma, and dermatofibrosarcoma protuberans. We acknowledge that some skin cancers are rare and slow growing, with features not always presenting in a typical manner. Claims settlements often take into account other factors and in many cases poor record keeping left the doctor vulnerable.
Claims relating to procedures
Claims relating to surgical excision of lesions, or treatment such as laser, all focussed on outcomes and scarring. Many patients reported they did not feel they had been adequately informed to consent for the procedure, or fully understood their options. Patients ended up with unexpected scarring from laser treatment and from procedures where a more extensive removal was done.
Factors leading to claims being settled were failure to obtain informed consent through discussion of risks and benefits, and failure to provide information about other options available.
Patient complaints: common themes
When we analysed the complaints reported by dermatologists seeking advice from us, there were some similar concerns to the claims, such as delayed diagnosis of cancer, but also some new themes.
More than 100 complaints were analysed, covering a wide range of concerns and reflecting the different areas in which dermatologists work. Complaints were received both about NHS work and in relation to procedures carried out in the private sector.
In relation to dermatologists, complaints included the following:
- burns sustained during cautery
- scarring
- removal of incorrect lesion
- delayed diagnosis of cancer or dermatological condition
- incorrect diagnosis
- surgical technique for lesion removal
- medication prescribing
- manner and attitude
- failure to review in person
- patient dissatisfaction with outcomes (specifically acne treatment)
A significant proportion of complaints clinically related to acne treatment, with parents making complaints on behalf of their children. Side effects from isotretinoin, including effects on growth and dry eyes, featured highly in complaints, although not claims, as most were NHS patients. There were also cases where blood tests were delayed when patients were either due to be starting isotretinoin or when already taking the medication.
Eczema complaint themes included a lack of verbal advice regarding potential side effects of oral and topical steroids and patients not fully understanding the reason for a tapering dose. In other complaints, patients reported they were not advised to taper the dose.
In other notable themes, concerns were raised regarding the appropriateness of history taking, specifically in relation to relevant sexual history and examination appropriateness. This highlights the importance of explaining to patients why information may be relevant clinically, even if it may feel inappropriate to a patient. Where a skin condition may affect an intimate area of the body, appropriate chaperone arrangements must be made in accordance with GMC guidance.
Regulatory (GMC) and disciplinary cases: common themes
We are aware of the immense pressure and stress that many doctors go through during these investigations. We always aim to provide members with tailored care and expert support.
GMC cases and hospital disciplinary matters have followed concerns raised by patients, relatives, or colleagues, both senior and junior. There was a mix of clinical and non-clinical concerns. Some investigations related to more than one concern. The themes identified included:
- Probity issues, for example:
- conducting private practice in NHS time
- access to records after leaving a trust - Inappropriate personal behaviour or misconduct, such as inappropriate comments made to patients
In the absence of representation by a defence organisation, the cost of instructing a solicitor to assist with a regulatory matter can be significant. Clinicians should ensure they have indemnity for all work being undertaken, as this review highlighted cases where doctors could not be assisted due to not being fully covered for their private work.
No one clinical theme was prevalent within this case type, but prescribing themes were noted with regards to ensuring patients fully understood the treatment options and risks associated with specific medication options. Specific concern for isotretinoin was noted and clinicians are reminded to follow local and national guidance and consider age-appropriate information is given to patients to ensure informed consent and shared decision-making.
Inquests: common themes
Assistance for inquest statements is rare for dermatologists, with only five cases identified relating to dermatological conditions between 2020 and 2024. An inquest is a factfinding exercise that is conducted by the coroner, and, in some cases, in front of a jury. The purpose of an inquest is to find out who died – when, where, how, and in what circumstances. Further information about what happens at an inquest and what to expect can be found in our essential guide to inquests.
Most inquests conclude uneventfully, but if a clinician is criticised by the coroner during the inquest or in the conclusion, then it is usually necessary to self-refer to the GMC to fulfil the obligations imposed by Good Medical Practice
It is therefore important to seek early support from your defence organisation if you are asked to provide a statement for an inquest for any patient you have treated, either on the NHS or privately.
Aesthetic and cosmetic considerations
Within the cases examined, there were fewer cases than expected resulting from aesthetic treatments. This may be for a number of reasons, including reporting delays (such as patients complaining or bringing a claim after the event) and the fact that practitioners other than dermatologists also undertake cosmetic procedures.
However, what we do know is that cosmetic and aesthetic medicine is an ever-changing area of private practice, where procedures and technologies continue to develop rapidly. Patients are becoming increasingly aware of their options – ranging from botox, non-permanent fillers, and cryotherapy, through to facial peels and microdermabrasion – and a growing number of clinicians are undertaking these types of procedures.
Such procedures may appear minor, and low risk, however each requires adequate training and comes with its own risks, which patients do not always appreciate. One of the main medicolegal risks, however, is managing expectations. Patients expect an improvement in appearance, and not seeing the results they hoped for can result in challenging conversations, complaints, or poor reviews. Getting the consent process right is vital.
This is in accordance with the themes detected among other non-aesthetic dermatological cases.
Dr Sarah Townley, Deputy Medical Director at Medical Protection, has written the following article that will interest anyone considering starting aesthetic practice, along with those who want to ensure their practice accords with the expected standards.
Dermatology in the UK: top tips to minimise risk
Please note this is not an exhaustive list of recommendations, but key learning points from our analysis.
- Remember that accurate and clear documentation, which may need to be relied on years after the event, is the cornerstone of any medicolegal defence.
- You may be asked to write a statement about your practice months or even years after an event. Ensure that your contemporaneous record keeping allows you to give a comprehensive account of your involvement, even if you cannot remember the patient concerned.
- Some complaints brought by patients or relatives follow dissatisfaction with the manner and attitude they experience during the consultation. Pay attention to how you may be perceived during discussions and ensure time is taken to explain the situation and answer any questions – especially considering the cosmetic outcome expectation of the patient.
- Discuss the possible benefits and risks of all potential dermatological treatments. Consider what is most important to that individual, taking into account their current employment and lifestyle. Ensure that the potential risks and benefits of each option has been discussed and that patients have realistic outcome expectations.
- Explain frequent and serious complications, and the implications for the individual patient if these occurred.
- Provide patients with additional resources, such as leaflets and websites, to assist a patient’s understanding of their condition and the treatments being offered.
- Double check that the information has been understood and allow the patient sufficient time to consider the information and reach a decision.
- Understand your patient’s concerns and expectations, and address any queries they may have. This is especially the case where aesthetic outcomes are important for the patient or where a patient may have an unrealistic belief about the outcome that can be achieved.
- Demonstrate empathy in your consultations and show your patient that they are the focus of your attention.
- Where costs are involved, your patients should be given clear information about all the costs involved and what their rights are to refunds or return of deposits if they change their mind after they have paid some or all of the costs.
- Ensure you are fully indemnified to carry out the full scope of your practice in the UK.
About the author
Dr Emma Green is a medicolegal consultant with a career in emergency medicine before joining Medical Protection in 2016. She returned to the frontline to assist during the COVID-19 pandemic. She has worked across a range of departments at Medical Protection, including claims, case handling, and more recently in underwriting.