Learning from cases: Anaesthesia
Post date: 13/06/2025 | Time to read article: 10 minsThe information within this article was correct at the time of publishing. Last updated 19/06/2025
Read this resource to:
• understand the claims environment in anaesthesia: Insights and lessons learned.
• receive tailored advice and key recommendations to help you reduce risks in the future.
Anaesthesia is a unique field, so the advice you receive needs to be equally specialised.
As a Medical Protection member, you benefit from more than 130 years of experience defending doctors and other healthcare professionals. That isn’t just a number – it’s more than 13 decades of specialist expertise that we use to protect you long into the future.
The team at Medical Protection, including medicolegal experts and cases and claims specialists, have delved into a huge range of anaesthetic cases to analyse the common reasons for claims and the different case types, to help keep you up to date with the current trends and provide insights into the anaesthesia claims and complaints landscape.
We hope you find this a useful source of guidance and advice, empowering you to protect yourself throughout your career.
Introduction
While complications resulting in claims following anaesthesia are rare, medicolegal cases are not uncommon due to the significant impact they can have on patients’ lives.
The majority of cases reported to us relate to elective procedures undertaken outside the NHS. Claims in anaesthesia can sometimes lead to large financial settlements because complications can result in serious and permanent loss of function, for example nerve damage from regional anaesthesia.
The value of the settled claim will often include compensation for care and loss of earnings if applicable, in addition to an award for the damage that resulted from a breach of duty. The value of each claim varies enormously with our highest anaesthesia total case payment considered in this analysis (including claimant damages, costs, and legal costs) being in excess of £3 million.
In addition, COVID-19 meant a significant change to the way in which many doctors worked, including severe disruption to elective surgery within the NHS. We also saw a large number of individuals contacting our medicolegal helpline for advice and support.
Issues arising as a consequence of COVID-19 included the prioritising of scarce resources, concerns over staffing levels, COVID-19 vaccinations (including in relation to doctors who did not wish to be vaccinated and also those who had fraudulently obtained vaccinations for themselves or their family ahead of schedule), management of patients who refused to wear a mask, and worries about personal risk of exposure. Medicolegal cases where COVID-19 is cited as a factor are ongoing and it is likely the impact will continue to be felt for some time.
As an anaesthetist, you work in complex and often pressured environments. We also know, following feedback from members, that experiencing a medicolegal case can be incredibly stressful. At Medical Protection, we want to share our knowledge, experience, and expertise with you so we can provide invaluable professional support.
Analysis
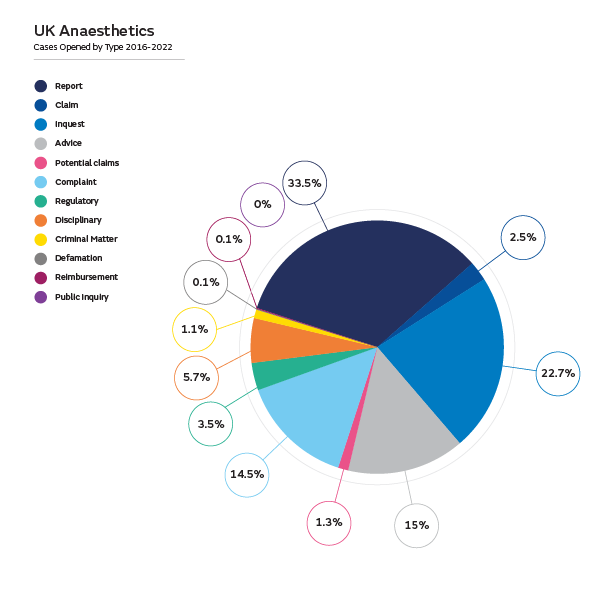
We have analysed the support we’ve provided UK- based anaesthetists and intensivists between 2016 and 2022 – in excess of 2,000 cases. In addition to providing advice and assistance in writing medical reports in over 700 of these cases, we have supported our members in relation to a total of over 1,100 situations, including:
- claims, as in demands for monetary compensation that embodies allegations of negligence
- potential claims, which are intimations from a claimant of a possible claim for compensation
- complaints
- General Medical Council (GMC) investigations
- local disciplinary procedures
- inquests.
By reviewing all the claims cases, including those defended, not pursued, and settled, we’ve identified some of the reasons that patients decide to take action against anaesthetists. Here you’ll also find some explanations of why claims are settled.
Claims: procedures and contributory factors
Dental Damage
The highest number of claims related to dental injury. This included claims for damage to crowns, veneers, and bridges, as well as native teeth.
Around half of these claims were not pursued by the claimant following our involvement. In claims that were defended or not pursued, the claimant’s dentition was assessed, including establishing the presence of crowns, veneers, and bridges, prior to anaesthesia, and the possibility of dental damage was clearly explained and fully documented. This enabled us to provide robust defences to claimant allegations.
Of those settled, the common themes included a failure to obtain a pre-operative history on the state of the patient’s dentition and a failure to warn of and document the risks of dental damage.
In some cases, there was evidence that dental damage occurred after the claimant had recovered from anaesthesia, for example, during eating. As a result of good preoperative documentation detailing a clear assessment of dentition, we were able to refute these claims.
Spinal and epidural anaesthesia
The majority of the claims were brought in relation to alleged neurological damage sustained at the time of the procedure, which led to ongoing and persisting neurological symptoms, such as paraesthesia and weakness to one or more limbs. The highest claim payment totalled over £3 million.
Factors leading to claims being settled were failures to obtain informed consent through discussion of risks and benefits, and failure to provide information about other options available, particularly where spinal or epidural anaesthesia were being utilised primarily for the purpose of postoperative pain relief.
Nerve damage due to malpositioning
Some claims contained allegations relating to nerve damage occurring as a result of malpositioning of the anaesthetised patient, inappropriately applied compression stockings, or sequential compression sleeve devices. These claims were often also brought against other theatre staff members, including operating department practitioners and the operating surgeon. The majority of these claims were ultimately discontinued against our anaesthetist members following assistance from us.
The approach taken by solicitors acting for the claimants in many of these cases was that even if the anaesthetist was not the practitioner positioning the patient, they held overall responsibility. While we have successfully disputed that this is not necessarily the case, we would continue to urge anaesthetists to be mindful of a patient’s position and the padding of pressure areas, as it is understandably stressful to be the recipient of a letter alleging negligence under these circumstances.
Awareness during general anaesthesia
Medical Protection continues to see a very small number of claims in relation to accidental awareness, nearly always involving the use of muscle relaxants. Claimants experienced distress at the time of awareness and frequently post-traumatic stress disorders. All awareness claims were settled, with the highest total payment of over £36,000.
Patient complaints: common themes
When we analysed the complaints reported by anaesthetists seeking advice from us, there were some similar concerns to the claims, such as dental damage and complications relating to spinal anaesthesia, but also some new themes.
More than 300 complaints were analysed, covering a wide range of concerns and reflecting the different areas in which anaesthetists work. Complaints were received both about NHS work and in relation to procedures carried out in the private sector.
In relation to anaesthesia, complaints included the following:
- Poor communication, including rudeness and inappropriate remarks made to patients during preoperative assessment and in the anaesthetic room. Complaints by colleagues relating to the manner and attitude displayed towards other staff members were also made.
- Inadequate postoperative analgesia.
- Ineffective spinal or epidural anaesthesia and complications of postdural puncture headache, haematoma, infection, and neural damage.
- Painful or repeated attempts at cannulation.
- Failure to provide adequate sedation leading to anxiety or discomfort.
- Failure to obtain informed consent or discuss options with the patient, for example general anaesthesia versus spinal.
- Administration of medications that the patient had said they did not want (such as opioids) without further discussion with the patient to explore their concerns.
- Failure to act on abnormal blood results preoperatively, leading to intraoperative or postoperative complications.
For critical care medicine, complaints often related to discussions with relatives, including allegations of poor communication with respect to treatment withdrawal or, in some cases, complaints that treatment withdrawal was not discussed with relatives at all. Other complaints included allegations of unnecessary and excessive use of sedation.
Complaints specifically relating to pain medicine included those relating to a lack of empathy shown during consultations and inappropriate comments by the anaesthetist. A number of complaints related to delays in providing treatment, misdiagnosis of the source of pain, and continuation of pain after treatment.
Regulatory (GMC) and disciplinary cases: common themes
We are aware of the immense pressure and stress that many doctors go through during these investigations. We always aim to provide members with tailored care and expert support.
GMC cases and hospital disciplinary matters have followed concerns raised by patients, relatives, or colleagues, both senior and junior. There was a mix of clinical and non-clinical concerns. Some investigations related to more than one concern or a series of serious clinical incidents. The common themes were:
- Performance concerns, such as technical skills, including poor airway management, clinical judgement, prescribing, and communication.
- Probity issues, for example:
- not reviewing patients prior to a theatre list
- leaving anaesthetised patients unattended or with an untrained colleague
- prescribing for family members, colleagues, or self
- being unavailable when on call or refusal to attend to a patient when requested
- conducting private practice in NHS time
- providing fraudulent information on job applications or in appraisals
- working as a locum while on sick leave from the employing trust
- retrospectively amending medical records or the anaesthetic chart.
- Inappropriate personal behaviour or misconduct, such as inappropriate comments made to patients, bullying, and harassment of colleagues.
- Health issues, including alcohol or drug misuse, and the theft of drugs from hospital premises. In addition, a small number of cases arose where concerns had been raised about potential ill-health or drug misuse in other colleagues, and these concerns were not adequately addressed or escalated. It is worth noting that GMC guidance requires a clinician to seek advice on any concerns they may have regarding the fitness to practise of colleagues.
In the absence of representation by a defence organisation, the cost of instructing a solicitor to assist with a regulatory matter can be significant. For example, the costs incurred on one of the regulatory cases considered during this time period was in excess of £100k. This figure may be substantially more if other case types are also involved, such as disciplinary action or an inquest.
Inquests: common themes
We assisted members in writing statements and attending coroner’s inquests on over 500 occasions between 2016 and 2022. An inquest is a factfinding exercise that is conducted by the coroner and, in some cases, in front of a jury. The purpose of an inquest is to find out who died – when, where, how, and in what circumstances. Our essential guide about inquests gives further information about what to expect.
Our analysis identified the following themes:
- Blockage or disconnection of tracheostomy tubes, including difficulties in re-siting.
- Delayed or failed intubation, including ‘can’t intubate, can’t ventilate’ scenarios.
- Aspiration pneumonia, including, as a consequence, the incorrect placement of a nasogastric tube into the bronchial tree.
- Inadvertent arterial puncture when siting central lines.
- Sepsis.
- Hypoxaemia following induction of anaesthesia, leading to hypoxic brain injury or other complications.
- Pulmonary embolus.
- Intra-abdominal haemorrhage, including in Jehovah’s Witnesses who declined blood products – in this situation the coroner may give careful consideration to matters of consent and capacity.
- Deaths in the intensive care unit following surgery or admission from the emergency department.
Assistance was also given in relation to inquests touching on perioperative deaths as a result of haemorrhage, amniotic fluid embolism, eclampsia, sepsis, pulmonary embolism, and uterine rupture.
On a number of occasions, anaesthetists or intensivists were asked to produce a statement detailing their clinical rationale for declining to transfer a patient to the intensive care unit or to escalate the level of support that was being provided.
We have also advised on providing a statement where the anaesthetist was not the primary clinician involved. Usually, they had participated in resuscitation attempts taking place in hospital wards, CT scanner rooms, and the emergency department, and most or all of the clinicians involved were subsequently asked for a statement. In some cases, members were requested by the coroner to write a statement months or even years after the event in question.
Most inquests conclude uneventfully but if a clinician is criticised by the coroner during the inquest or in the conclusion, then it is usually necessary to self-refer to the GMC to fulfil the obligations imposed by Good Medical Practice, which states a doctor must inform the GMC without delay if they are criticised by an official inquiry.
Anaesthesia in the UK: top tips to minimise risk
Please note this is not an exhaustive list of recommendations but key learning points from our analysis.
- Whether administering general or regional anaesthesia, ensure your anaesthetic technique is regularly updated and in line with current best practice, such that it would be supported by your peers.
- Remember that accurate and clear documentation, which often may need to be relied upon years after the event, is the cornerstone of any medicolegal defence.
- Discuss the possible benefits and risks of all potential anaesthetic or treatment options. Consider what is most important to that individual, taking into account their current employment and lifestyle. Ensure that the potential risks and benefits of each option has been discussed.
- Explain frequent and serious complications, and the implications for the individual patient if these occurred. Explain what you would do to correct or manage complications. Explain what you would do to correct or manage complications.
- Double check that the information has been understood and allow the patient sufficient time to consider the information and reach a decision.
- Understand your patient’s concerns and expectations and address any queries they may have. This is especially the case in pain medicine, where a patient may have an unrealistic belief about the outcome that can be achieved.
- A thorough assessment of dentition should be documented clearly, along with an indication that the patient has been warned of the risk of dental damage.
- Individuals with risk factors for dental injury, the presence of loose teeth, dental restorations, or a difficult airway should be warned there is a greater probability of damage.
- Some complaints brought by patients or relatives follow dissatisfaction with the manner and attitude of their anaesthetist. Pay attention to how you may be perceived during discussions and ensure time is taken to explain the situation and answer any questions.
- Demonstrate empathy in your consultations and show your patient that they are the focus of your attention.
- If involved in decisions about withdrawal of treatment, ensure that those individuals close to the patient are involved where appropriate, and that they are communicated with respectfully and sensitively.
- If involved in declining to admit a patient to intensive care, or in reaching a decision made that it would not be in the patient’s best interests to escalate treatment, ensure your clinical rationale for the decision is clearly explained and documented.
- Be aware that you may be asked to write a statement, including in relation to claims, inquests, and complaints about your practice months or even years after an event, and ensure that your contemporaneous record keeping would allow you to give a comprehensive account of your involvement, even if you cannot remember the patient concerned.
- In the event you have concerns about either your own or your colleague’s fitness to practise (for example, for health reasons) you should seek advice and assistance.
- Where costs are involved, your patients should be given clear information about all the costs involved and what their rights are to refunds or return of deposits if they change their mind after they have paid some or all of the costs.
- Ensure you are fully indemnified to carry out the full scope of your practice in the UK.
About the author
Dr Heidi Mounsey is a medicolegal consultant and assists members in relation to many of the matters outlined in this booklet. She is a former anaesthetic registrar and is a Fellow of the Royal College of Anaesthetists. She joined Medical Protection in 2016.


