Dr Lynelle Govender, Senior Lecturer at the University of Cape Town discusses how the high and lows of being an intern can all affect your sense of wellbeing.
Imagine you’re an intern, and you’ve just finished your first year of internship. Fresh out of medical school, you worked your way through the big first-year rotations: internal medicine, surgery, obs and gynae, paediatrics. Look back on the year, what did it feel like. What were the highs and lows, what helped you cope with that shift from being a student to being a doctor, what made it even more difficult?
I sat down with a fellow doctor, and asked him to reflect on exactly that: “Draw me a graph of your first year of internship. Trace a line to mark the highs, and lows. What was that transition like.”
Here’s an idea of what we found:
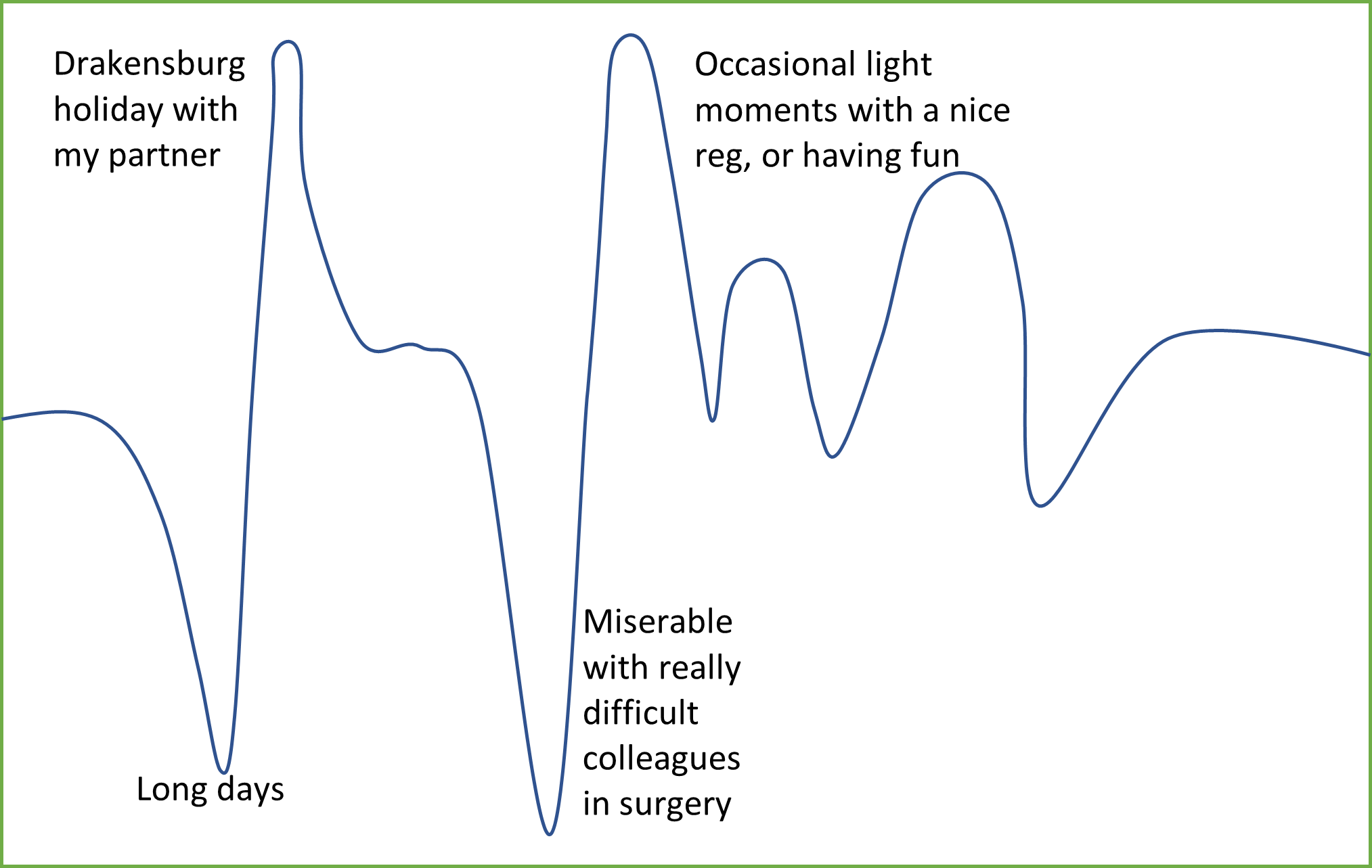 Figure 1: Transitional curve (Hurst et al. 2013) drawn by anonymous doctor, South Africa
Figure 1: Transitional curve (Hurst et al. 2013) drawn by anonymous doctor, South Africa
Can you relate to the graph above? Perhaps you’re going through it at the moment? The literature talks about this concept as transitional challenges. Transitional challenges are the particular changes faced by an individual when transitioning from one environment/career phase to another.
We all face transitional challenges repeatedly through our career, from pre-clinical medical student to being a clinical student working on the wards, from internship to community service, medical officer to registrar, and perhaps (one glorious day) to finally holding the role of the consultant. So, while this article focuses on the transition from medical student to intern, the concepts are applicable for any stage in your career.
Factors affecting wellbeing
Look at the graph again. Notice how the path goes up and down. It’s a bit of a rollercoaster, really. Think about those upswings and downswings as a gauge of well-being. Sometimes, things can feel absolutely horrible. You’ve just started as an intern, you don’t know the wards or the people and the workload is immense. On the contrary, sometimes it can feel okay, good even. You know the system, you’re confident with practical skills and you’ve made a few friends along the way. There are a number of the factors that affect well-being. So, what are these factors?
Team support
We have all been there. There are registrars who try to help you, versus registrars who disappear after the ward round, like smoke on the wind. The disappearing act doesn’t even begin to address the daily wear-and-tear when facing colleagues who are downright belligerent. A supportive team can make all the difference to your experience of the transition to internship, community service or even simply moving to a new clinical rotation.
Professional and practical confidence
There’s that moment when you start a rotation (or a career phase) and you have no idea what you’re doing. You’re confused and anxious. Then there’s that moment towards the end of rotation, where you manage most of your clinical duties with ease. Somewhere in between, while you weren’t watching too closely, you became confident in your professional identity and practical skills. That sense of confidence is what can propel you forward during a rotation, and supplies you with a much-needed boost in your general well-being.
Workload
Long working hours, negative patient outcomes, and the resultant fatigue is a double-edged sword. It leaves you exhausted, with little time or energy to spare for social activities and self-care, which is precisely what is needed in these times. In South Africa, clinical burdens can be exceptionally high. Going on-call can be particularly challenging; where workload, confidence and team dynamics can come to define the way a night plays out.
Coping
Below are some simple strategies and tools that can help, but this isn’t meant to downplay the complex and difficult reality. It is a complex period, with many factors at play. It’s a tough time. There’s no getting around it, but all is not lost. There is plenty that can be done to help you survive, and even thrive, during these transitional periods.
Reflect and self-care
Learning to critically reflect on your journey can be wonderful tool. It can help you reframe your experience, and maximise learning. Consider keeping a journal, or reflecting in whatever way suits you, to help you make meaning of your transitional experiences. Studies have shown that self-care behaviours such as exercise, high-quality sleep and meditation can help to cope with transitional challenges. Keep a close eye on yourself though, and seek help if you find yourself leaning on maladaptive coping mechanisms such as addictive substances.
Behaviours
Actively seek out support when you’re on the wards. Look around you. There are more people involved than you and your registrar. See yourself as a member of a team that includes nurses, and a multi-disciplinary team. Seek help when you are struggling.
In the face of difficult colleagues, try to speak up if possible. The ability to set down clear boundaries for yourself and those around you, will help you during these shifting times, and takes you one step closer to being an advocate for yourself and your patients.
Social support
The Beatles had it right. I get by with a little help from my friends. Simply talking to friends, family and partners about your experiences can help to alleviate your burden. Be honest with those around you, tell them about what happens in the wards, or when you are on call at night. Truthfully, the reality can be hard and harsh, but there is no reason for you to face it alone.
References
Hurst, C., Kahan, D., Ruetalo, M., Edwards, S. (2013) A year in transition: a qualitative study examining the trajectory of first year residents’ well-being. BMC Med Educ. 13(96).
http://doi.org/10.1186/1472-6920-13-96
Sturman, N., Tan, Z. & Turner, J. (2017). “A steep learning curve”: junior doctor perspectives on the transition from medical student to the health-care workplace. BMC Med Educ. 17(92).
http://doi.org/10.1186/s12909-017-0931-2
Need to talk to someone or want to find out how Medical Protection can support you? Simply visit the wellbeing hub which has information on how you can access confidential counselling, the wellbeing app, podcasts, webinars and more.