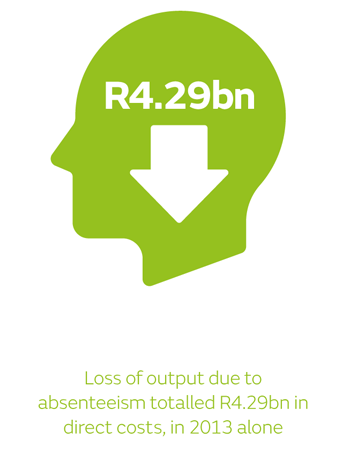
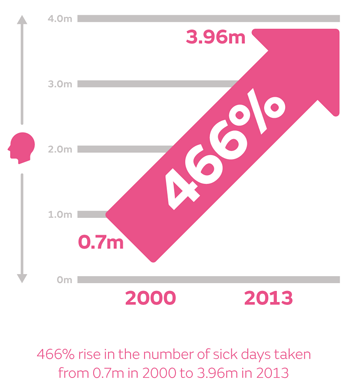
According to Occupational Care South Africa (OCSA) and Statistics South Africa, the abuse of sick leave is costing the South African economy between R12 billion to R16 billion a year.
OCSA estimates that there is an average of 15% of staff absent on any given day and that only one in three absent employees is genuinely physically ill. What is concerning is the fact that a great deal of poor medical certificate practice has been seen, and forgeries by patients (not the fault of the medical practitioner) have become increasingly common.
Sick leave - Managing the abuse
 This rise in sick leave abuse by employees means it has become increasingly common for disgruntled employers not only to institute disciplinary action, but also to lodge complaints with the HPCSA against medical practitioners for issuing medical certificates that do not strictly comply with the provisions of the HPCSA’s Ethical Rules of Conduct and/or being too generous in issuing medical certificates.
This rise in sick leave abuse by employees means it has become increasingly common for disgruntled employers not only to institute disciplinary action, but also to lodge complaints with the HPCSA against medical practitioners for issuing medical certificates that do not strictly comply with the provisions of the HPCSA’s Ethical Rules of Conduct and/or being too generous in issuing medical certificates.
Since 2007, there have been several dozen instances of medical practitioners being charged and found guilty of unprofessionalconduct related to poor medical certificate practice. The reported penalties imposed by the HPCSA have ranged from caution and reprimand to fines not exceeding R15,000. Clinicians should be familiar with the relevant statutory and ethical guidelines and requirements in respect of the issuing of valid medical certificates. This includes the provisions of section 23 of the Basic Conditions of Employment Act (Act No 75 of 1997), as well as the Rule 16 of the HPCSA’s Ethical Rules of Conduct.
The Basic Conditions of Employment Act (Act No 7 of 1997)
In terms of section 29(1) of the Basic Conditions of Employment Act, an employee is obliged to furnish a legitimate medical certificate if the employee is absent from work for more than two consecutive days or on more than two occasions during an eight-week period. Section 23 of the Act deals with proof of incapacity and outlines the requirements for legitimate and acceptable medical certificates qualifying an employee to be paid statutory sick leave.
In short, the medical certificate must state that the employee was unable to perform his or her normal duties because of illness (or an injury), and that this diagnosis is based on the professional opinion of the medical practitioner.
The medical certificate must be issued and signed by a medical practitioner or any other person who is certified to diagnose and treat patients, and who is registered with a professional council established by an act of parliament.
Ethical rules of conduct - The HPCSA
Further guidelines relating to the issuing of valid medical certificates as contemplated in section 23 of the Basic Conditions of Employment Act can be found in Rule 16 of the HPCSA’s Ethical Rules of Conduct.
In terms of Rule 16(1), a medical practitioner shall grant a medical certificate only if it contains the following information:
a. the name, address and qualification of such practitioner
b. the name of the patient
c. the employment number of the patient (if applicable)
d. the date and time of the examination
e. whether the certificate is being issued as a result of personal observations by such practitioner during an examination, or as a result of information which has been received from the patient and which is based on acceptable medical grounds
f. a description of the illness, disorder or malady in layman’s terminology with the informed consent of the patient: provided that if such patient is not prepared to give such consent, the practitioner shall merely specify that, in his or her opinion based on an examination of such patient, such patient is unfit to work
g. whether the patient is totally indisposed for duty or whether such patient is able to perform less strenuous duties in the work situation
h. the exact period of recommended sick leave
i. the date of issue of the certificate of illness
j. the initials and surname in block letters and the registration number of the practitioner who issued the certificate.
In terms of Rule 16(2), read with Rule 15, medical certificates are official documents and must be personally and originally signed by a medical practitioner next to his or her initials and surname, which must be printed or written in block letters. The signature must be legible.
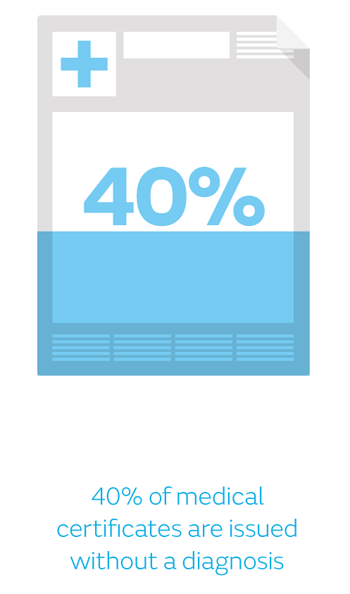
Rules 16(1)(e) to 16(1)(g) stipulate that a medical certificate should only be issued on the basis of a proper medical examination and diagnosis of a patient, and not on the mere observation of a patient.
 Rule 16(1)(e) refers to those occasions where, for example, the patient has been off sick from work on Monday and Tuesday and then on Wednesday consults with a medical practitioner and informs the practitioner that he or she has been ill since Monday, and requires a medical certificate in respect of the entire week. In these circumstances, a medical practitioner may only retrospectively book the patient off for Monday and Tuesday if, in his or her professional opinion, the patient was actually unable to perform his or her normal duties during the backdated period.
Rule 16(1)(e) refers to those occasions where, for example, the patient has been off sick from work on Monday and Tuesday and then on Wednesday consults with a medical practitioner and informs the practitioner that he or she has been ill since Monday, and requires a medical certificate in respect of the entire week. In these circumstances, a medical practitioner may only retrospectively book the patient off for Monday and Tuesday if, in his or her professional opinion, the patient was actually unable to perform his or her normal duties during the backdated period.
An example may be when a patient presents with an infectious disease, the symptoms of which only became visible on Wednesday, but which would have caused the patient to feel ill during the preceding incubation period. In these circumstances, it is essential that the medical practitioner clearly indicates on the certificate that he or she was merely informed that the patient was ill on Monday and Tuesday, and that the conclusion was not based on personal observations made by the practitioner. With the exception of this example, the issuing of backdated medical certificates would generally constitute unprofessional conduct.
Certificates of medical attendance
A distinction should be drawn between medical certificates that recommend a period of sick leave, and certificates of medical attendance. A certificate of medical attendance merely serves as a confirmation that the practitioner saw the patient or was informed by the patient that the patient was ill – it is not considered to be a valid medical certificate.
Extending sick leave
 In the event that a patient requests an extension of the originally allocated sick leave, the medical practitioner should insist on conducting a follow-up consultation with the patient and should issue an additional medical certificate. A medical practitioner may not extend the initial period of sick leave and issue an additional medical certificate without having consulted with and physically examined the patient.
In the event that a patient requests an extension of the originally allocated sick leave, the medical practitioner should insist on conducting a follow-up consultation with the patient and should issue an additional medical certificate. A medical practitioner may not extend the initial period of sick leave and issue an additional medical certificate without having consulted with and physically examined the patient.
The medical certificate must be an original document. Extending sick leave telephonically, having the patient amend the original medical certificate, or faxing or emailing medical certificates is unethical and could lead to a finding of unprofessional conduct.
Rule 16(1)(f) states that the medical practitioner should give a description of the illness, subject to the patient giving his or her informed consent to the disclosure. In terms of the Guidelines of Good Practice issued by the HPCSA regarding patient confidentiality, medical practitioners must obtain express verbal or written consent where patients may be personally affected by the disclosure.
It is important to always obtain the patient’s express informed consent before disclosing the diagnosis in a medical certificate, particularly so if the nature of the diagnosis could embarrass or prejudice the patient. If the patient is not prepared to give such consent, the medical practitioner shall merely specify that, in his or her opinion based on an examination of such patient, such patient is totally indisposed for duty or is able to perform less strenuous duties in the work situation.
Confidentiality - The employer's rights
With regards to patient confidentiality, a general misconception exists that an employer may not contact a medical practitioner to validate a medical certificate, as this would constitute a breach of patient confidentiality. This is not the case.
Although a medical practitioner is prohibited from disclosing any confidential information regarding the patient’s medical condition without their specific consent, a medical certificate would not constitute privileged information should the patient submit it as proof of their absence due to illness.
The employer, therefore, has a right to investigate the validity of the certificate to confirm that the patient did indeed visit the medical practice on the date stated on the certificate, as well as to confirm the actual dates booked off.
Staying safe
In view of the widespread fraud involving medical certificates, medical practitioners should take reasonable steps in order to keep their certificates in a safe place. Should it be found that a patient misappropriated a pad of medical certificates left lying around in the practitioner’s practice in a negligent or irresponsible manner, such a practitioner may be been found guilty of unprofessional conduct by the HPCSA. In the event of a practitioner becoming aware of fraudulent medical certificates being issued in the name of the practitioner, it is advisable to report the matter to the South African Police Services.
A medical certificate may only be issued if the patient is truly medically unfit to perform his or her normal duties: they may not be issued for routine check-ups, examinations, tests, collecting medicine from the pharmacy, or visits to specialist medical practitioners. Medical practitioners often come under considerable pressure from patients, especially those who have been patients of a particular practitioner for many years, to issue medical certificates when it is not strictly indicated.
Medical practitioners should resist these pressures and issue medical certificates strictly on merit at all times. Although not specifically mentioned in the Ethical Rules of Conduct, medical practitioners should also be careful not to issue medical certificates in respect of medical conditions that fall outside their scope of practice and expertise.